Abstract
Introduction
Cardiac involvement of amyloid is a critical determinant of prognosis for light chain (AL) amyloidosis. Predictive survival outcomes are primarily determined by the Mayo Clinic prognostic scoring system which incorporates cardiac biomarkers and serum free light chain assay. Diagnosis of cardiac AL involvement is often established by fibrillary typing on an endomyocardial biopsy (EMB). However, prognostic data from detailed tissue examination beyond fibrillary typing are lacking. The purpose of this study was to evaluate histopathological findings from EMB involved by AL, establish a cardiac-specific biopsy scoring system and correlate these findings with clinical outcomes.
Methods
Patients with AL amyloidosis diagnosed between 2008 and 2016 were retrospectively reviewed to identify ones with cardiac AL involvement. Consecutive EMB samples involved by AL were evaluated by a pathologist with expertise in cardiac AL who was blinded to clinical data. A Fibrosis Score (FS) was determined by calculating the collagen polarization area expressed as a percentage of total area examined in each biopsy fragment. Similarly, an Amyloid Score (AS) was calculated as the green birefringent amyloid area expressed as a percentage of the total area examined. A composite cardiac injury score (CCIS) was then generated using the sum of the FS and AS.
The primary outcome of interest was the development of a cardiovascular adverse event (CVAE) during the course of treatment for AL. CVAEs were defined according to the CTCAE v4.03: heart failure (HF), arrhythmia requiring treatment, acute coronary syndrome (ACS) and venous thromboembolic event (VTE). Need for implantable cardiac device (i.e. pacemaker or defibrillator) and orthotopic heart transplant were also captured.
Results
Sixty-two patients with cardiac AL amyloidosis were identified. Twenty-nine had biopsy-proven cardiac involvement and 33 had highly-suspected cardiac involvement based on cardiac biomarkers, imaging, and other sites of biopsy-proven AL amyloidosis.
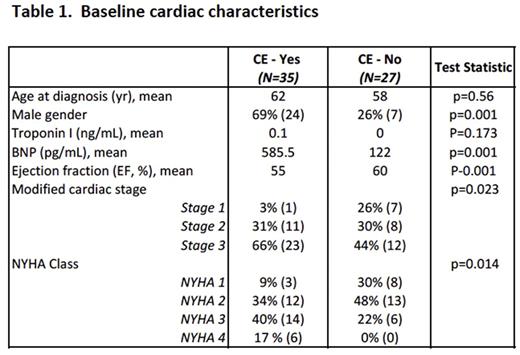
The median follow-up was 38.1 months. During the course of treatment, 56% (n=35) experienced at least one CVAE. A total of 66 events occurred including HF (n=19), arrhythmia requiring treatment (n=22), ACS (n=8), VTE (n=6), need for an implanted device (n=9) and orthotopic heart transplantation (n=2). At baseline, patients experiencing a CVAE were more likely to be male (P=.001), have higher brain natriuretic peptide (BNP) levels (P=.001), higher modified cardiac stage1 (P=.023) and higher New York Heart Association (NYHA) class (P=0.014) (Table 1). The majority of patients (84%) received bortezomib-based chemotherapy with the remaining receiving melphalan or immunomodulatory-based therapy. 56% received consolidative autologous hematopoietic cell transplantation (AHCT).
Among the 29 patients with biopsy-proven cardiac AL involvement, 18 (62%) had at least one CVAE. The median CCIS was higher is patients experiencing a CVAE during the course of treatment compared with patients not experiencing a CVAE (12.39 vs. 5.46, P=0.04). By multivariate analysis, a CCIS of ≥ 5 was associated with development of CVAE compared with a CCIS of <5 (OR=4.61, 95% CI 1.13-18.75, P=0.04). Other variables evaluated and not found to be predictive of CVAEs included gender, chemotherapy administered, and AHCT.
There was no associated between CCIS and time to disease progression. The study was underpowered to evaluate CCIS and overall survival since only 8 patient deaths occurred in patients with available EMB samples.
Conclusions
Cardiovascular adverse events are common in patients with cardiac AL amyloidosis. Our results indicate an association between higher composite cardiac injury score derived from endomyocardial biopsy tissue involved by AL amyloidosis and the development of CVAE during the course of treatment. These data may be helpful to stratify patients into a higher risk group prompting closer cardiac monitoring during treatment. These findings warrant further analysis with larger sample sizes for developing pathologic prognostic tools to predict clinical outcomes in patients with cardiac AL amyloidosis.
References
1. Induction Therapy with Bortezomib Followed by Bortezomib-High Dose Melphalan and Stem Cell Transplantation for AL Amyloidosis: Results of a Prospective Clinical Trial. Sanchorawala et al . Biol Blood Marrow Transplant, 21 (2015) 1445-1451
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal